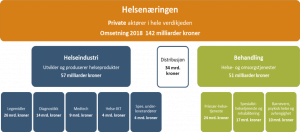
Ny rapport: Helsenæringens verdi 2019

Rapporten gir innsikt i en næring som i 2018 omsatte for 142 milliarder kroner.
Helsenæringen er en dobbel mulighet for Norge: næringen kan løse mange av våre helse- og omsorgsutfordringer de neste tiårene og samtidig bli en av våre største næringer, med eksport til et globalt marked.
Den fjerde Menon-rapporten om helsenæringens verdi går nærmere inn på tallene bak disse mulighetene.
Viktige funn i rapporten:
- Omsetningen i helsenæringen var på 142 milliarder kroner i 2018.
- Helsenæringen er global og bedriftene i industrien vender seg mot internasjonale markeder tidlig.
- Helserelatert eksport var på over 23 milliarder kroner i 2018.
- Næringen er avhengig av ny kapital i utviklingsløpet: fire av ti bedrifter hentet inn ny egenkapital i 2018.
- Helseindustrien er en gründernæring: en av ti bedrifter er i gründerfasen.
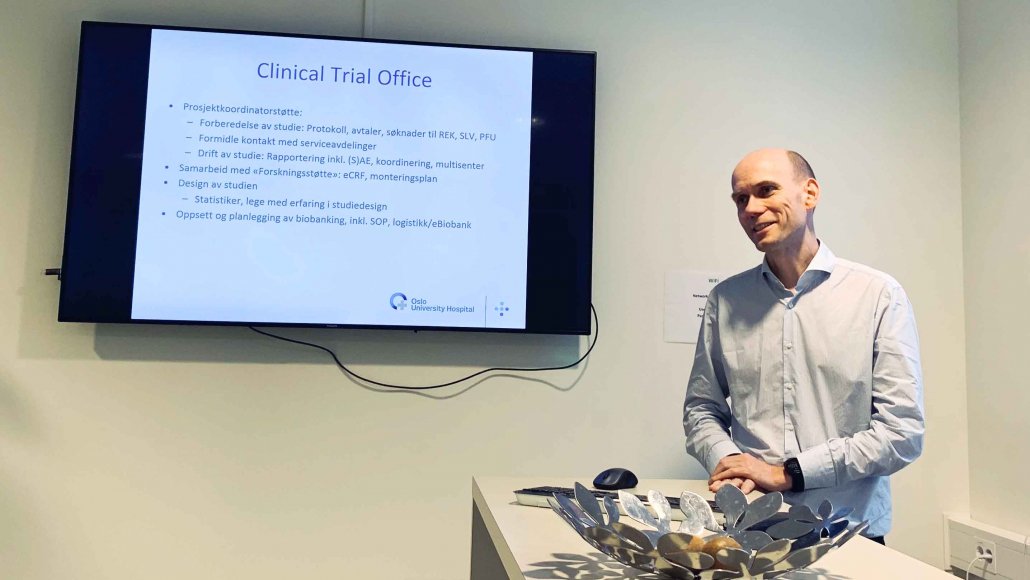
- Det er en svært FoU-intensiv næring, der spesielt kliniske studier er viktig. Likevel falt antall søkte industrifinansierte kliniske studier fra 175 i 2000 til bare 72 i 2018.
Hjemmemarked og risikokapital
Mye er på plass for norsk helsenæring, men i følge Menon mangler to ting: Det ene er et stort hjemmemarked med kompetente, krevende lokomotivkunder. Det andre er langsiktig risikokapital for raskere utviklings-, kommersialiserings- og vekstprosesser.
– Det som er litt fint med de to utfordringene, er at de henger tett sammen. Lykkes man med det første, er sjansene store for å lykkes med det andre, understreket Erik W. Jakobsen, Managing Partner i Menon Economics, under lanseringen.
En internasjonal næring
Under lanseringsarrangementet i Næringslivets Hus i Oslo 25. april, ble enda et utspill lansert:
Innovasjon Norge med samarbeidspartnere, blant annet Oslo Cancer Cluster, lanserte en global strategi for norsk helseindustri. Den heter “Pioneering sustainable health”.
– Helse er en «born global næring», og det må vi nå utnytte. Vi må gjøre norske helseløsninger bedre kjent internasjonalt. Visjonen er å tredoble norsk helseindustri innen 2030, sa Hans Eirik Melandsø, sektoransvarlig helseindustri i Innovasjon Norge.
Næringsminister Torbjørn Røe Isaksen (H) var også med på arrangementet og presenterte hovedpunkter fra Regjeringens stortingsmelding om helsenæringen, som ble lansert 5. april. Stortingsmeldingen kan du lese på nettsidene til Regjeringen.
Hvordan kan norsk helsenæring lykkes i å ta en internasjonal posisjon? Det er et nøkkelspørsmål som går igjen i rapporten fra Menon, Stortingsmeldingen om helsenæring og posisjonen “Pioneering sustainable health”.
– Vi ligger i et helsenæringsnabolag. Sverige er store, Danmark er veldig store. Det er en stor fordel at “the Nordic region” er kjent for og har kompetanse på dette fra før. Det må vi utnytte bedre, sa Torbjørn Røe Isaksen.

Ordskifte mellom stortingsrepresentant Ingvild Kjerkol (Ap) og næringsminister Torbjørn Røe Isaksen (H). De var enige om behovet for bedre samarbeid mellom private og offentlige aktører.
Offentlig-privat kulturendring
En bedre kultur og insentiver for samarbeid er et annet viktig poeng når norsk helsenæring diskuteres.
– For mange private aktører møter skepsis, stengte dører og problematisering når de forsøker å samarbeide med det offentlige. Vi må ha tjenester som slipper næringen til, slik at næringen også kan forstå hva som skal til, sa Torbjørn Røe Isaksen.
– Det jeg savner i Stortingsmeldingen, er klyngene og TTO-ene. Når vi ser på Menons vekstrater for industrien, ser vi at det er noe som fungerer bra. Framover bør vi gjøre mer av det som fungerer, og ikke bare finne på nye virkemidler. I en videre strategi bør klyngenes rolle få en større plass og utvikles, sa stortingsrepresentant Ingvild Kjerkol (Ap).
Du kan lese hele rapporten her:
Lenker til Menon-rapportene om helsenæringens verdi fra tidligere år:
Menon-rapporten utgis av:
Andre relevante saker: