The Incubator Labs are expanding

The laboratories at Oslo Cancer Cluster Incubator are expanding to meet increasing demand from members.
Oslo Cancer Cluster Incubator has recently converted three offices into new laboratories to accommodate the rising demand from their members.
From the opening in 2015, the laboratories in the Incubator have been a great success. Several of the start-ups have expanded their work force and require more offices and lab space.
The new laboratory is jointly occupied by Zelluna Immunotherapy and the Department of Cellular Therapy (Oslo University Hospital). The Institute for Energy Technology and Arctic Pharma have also expanded their laboratories with an extra room each.
The laboratories are now running at full capacity, but there is some space available in the shared labs. Some of the members of the Incubator offer their services to outside companies who are in need of getting lab work done.
“Our ambition is to grow the Incubator Labs further into the new Innovation Park next door.” Bjørn Klem, General Manager
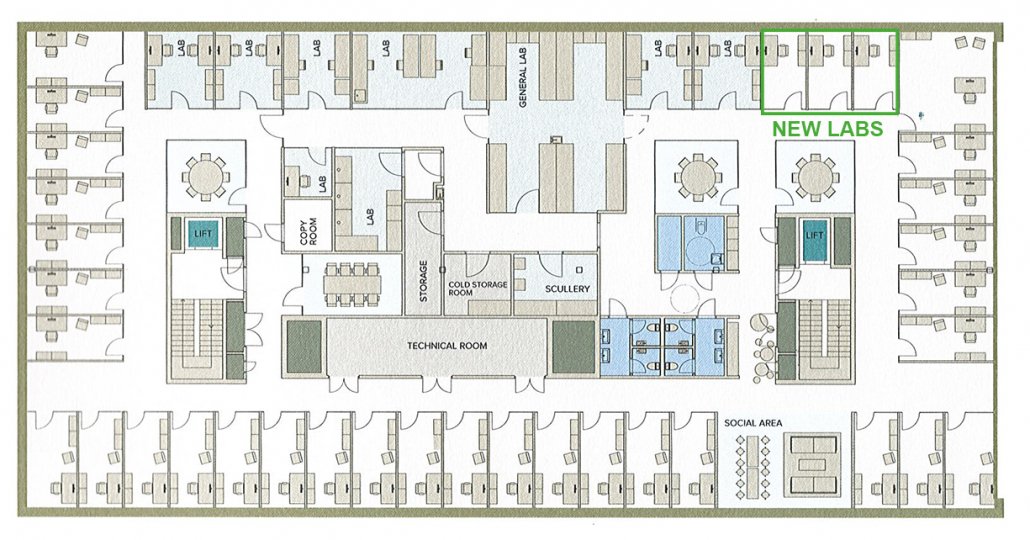
The Incubator occupies over 550 square meters. Offices have been converted into labs to meet the growing interest from the members.
A unique model
The Incubator Labs follow a unique model, which offers both private laboratories and fully equipped shared laboratories. The private laboratories are leased with furniture, water supply, electricity and ventilation. The companies bring their own equipment depending on their needs.
Shared laboratories, including a bacteria lab, a cell lab and wet lab, are leased including basic equipment with the opportunity for companies to bring their own if shared by all tenants. All laboratories share the common support facilities including a cold room for storage, a laundry room, and storage room including cell tanks and nitrogen gas.
“This model of a shared laboratory is very unusual,” said Janne Nestvold, Laboratory Manager at the Oslo Cancer Cluster Incubator.
The advantage of working in a shared lab is that companies can avoid the costs and limitations associated with setting up and managing a laboratory. A broad range of general equipment, including more advanced, analytical instruments, are provided by the Incubator.
”It would be too expensive for a small company to buy all this equipment themselves.” Janne Nestvold, Laboratory Manager

The Department of Cellular Therapy (Oslo University Hospital) are one of the members using the shared lab. Photograph by Christopher Olssøn
Open atmosphere
The laboratories have an open and light atmosphere. Large windows provide ample lighting and all spaces are kept clean and tidy. The halls are neatly lined with closets and plastic containers for extra storage.
The general mood is calm and friendly. Nestvold communicates daily with the users about changes, updates and improvements, which sets an informal tone. Thanks to monthly lab meetings, the users are also involved in the decision-making process. The companies often work side-by-side or in teams, fostering collaboration rather than competition. There is therefore a strong workplace culture based upon flexibility and mutual respect.
The companies often work side-by-side or in teams, fostering collaboration rather than competition.
Nestvold also ensures that the high demands on the infrastructure of the laboratory are met. She has put agreements in place to facilitate the members’ needs, such as the washing of lab coats, pipette service and shipping packages on dry ice. With all these services included, the Incubator Labs are attractive for researchers and companies to carry out their cancer research.
Over the years, Nordic Nanovector, OncoInvent, Targovax, Intersint, OncoImmunity have conducted research in the laboratories. Now, Arctic Pharma, the Department of Cellular Therapy (Oslo University Hospital), GE Healthcare, the Institute for Energy Technology, Lytix BioPharma, NorGenotech, Ultimovacs and Zelluna Immunotherapy are using the Incubator Labs to develop their cancer treatments.
- For more information about the Incubator Lab, get in touch with Janne Nestvold.