SINTEF to develop methods in immuno-oncology

SINTEF and Catapult Life Science are looking for new partners to develop methodology for cancer immunotherapy.
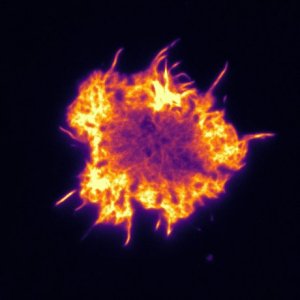
“We want to develop methods within immunotherapy, because this is currently the most successful strategy for improving cancer treatments and one of the main directions in modern medicine,” says Einar Sulheim, Research Scientist at SINTEF.
The Norwegian research organization SINTEF is an Oslo Cancer Cluster member with extensive knowledge in characterisation, analysis, drug discovery and development of conventional drugs.
The new project on methodology for cancer immunotherapy recently started in April 2019 and is a collaboration with Catapult Life Science, a new Oslo Cancer Cluster member. The aim is to help academic groups and companies develop their immunotherapy drug candidates and ideas.
Help cancer patients
Ultimately, the main aim is of course that the project will benefit cancer patients. Immunotherapy has shown to both increase life expectancy and create long term survivors in patient groups with very poor prognosis.
“We hope that this project can help streamline the development and production of immunotherapeutic drugs and help cancer patients by helping drug candidates through the stages before clinical trials.” Einar Sulheim, Research Scientist at SINTEF
Develop methodology
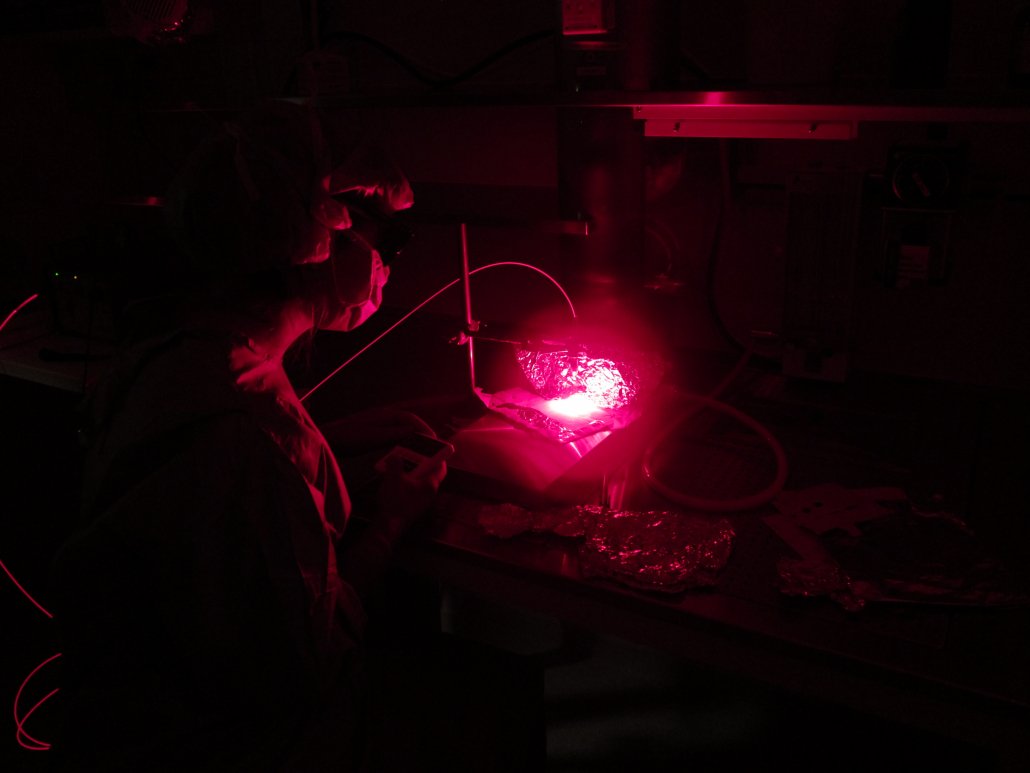
The project is a SINTEF initiative spending NOK 12,5 million from 2019 to 2023. SINTEF wants to develop methodology and adapt technology in high throughput screening to help develop products for cancer immunotherapy. This will include in vitro high throughput screening of drug effect in both primary cells and cell lines, animal models, pathology, and production of therapeutic cells and antibodies.
Bridging the gap
Catapult Life Science is a centre established to bridge the gap between the lab and the industry by providing infrastructure, equipment and expertise for product development and industrialisation in Norway. Their aim is to stimulate growth in the Norwegian economy by enabling a profitable health industry.
“In this project, our role will be to assess the industrial relevance of the new technologies developed, for instance by evaluating analytical methods used for various phases of drug development.” Astrid Hilde Myrset, CEO Catapult Life Science
A new product could for example be produced for testing in clinical studies according to regulatory requirements at Catapult, once the centre achieves its manufacturing license next year.
“If a new method is intended for use in quality control of a new regulatory drug, Catapult’s role can be to validate the method according to the regulatory requirements” Myrset adds.
SINTEF and Catapult Life Science are now looking for partners.
Looking for new partners
Einar Sulheim sums up the ideal partners for this project:
“We are interested in partners developing cancer immunotherapies that see challenges in their experimental setups in terms of magnitude, standardization or facilities. Through this project, SINTEF can contribute with internal funding to develop methods that suit their purpose.”
Interested in this project?
- More information and contact details on SINTEF’s project webpage
- Have a look at the webpage of Catapult Life Science