2,4 million euros for digital health innovations

Oslo Cancer Cluster has awarded EU funding of 2,4 million euro to companies that want to digitalise the medical sector.
What if the medical and technological sectors could join forces so that patients could receive more precise diagnosis and treatment? Imagine the products that could be created, the costs that could be saved and the lives that could be improved. This was the idea behind the EU-funded project DIGI-B-CUBE, which was coordinated by Oslo Cancer Cluster for the last three years.
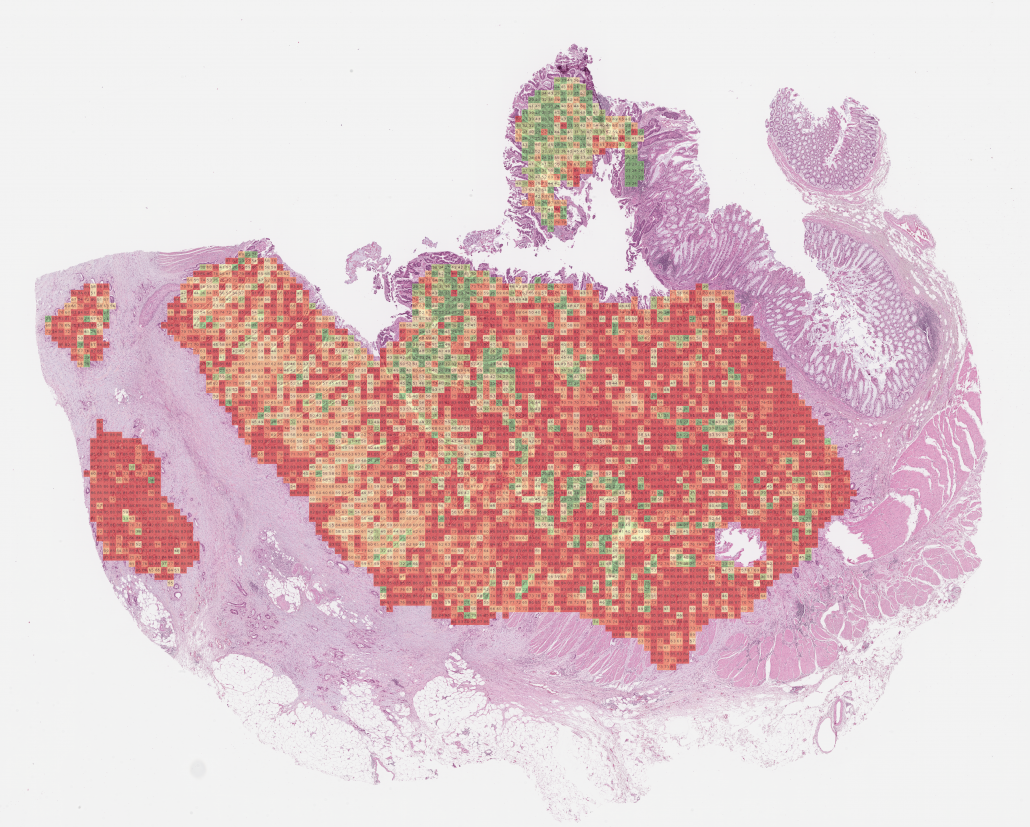
“We need to create collaborations between people working in medicine and people working in tech, so they can develop innovative solutions to handle health data or analyse medical images. This can lead to faster, more precise diagnosis, and ultimately advance precision medicine in cancer,” said Ketil Widerberg, general manager of Oslo Cancer Cluster.
Better diagnostics with tech
Simply explained, DIGI is short for digitalisation and B-CUBE is short for bio-imaging, bio-sensing and bio-banking. All three Bs are important tools in medical research and diagnosis, especially in personalised medicine.
The goal of DIGI-B-CUBE was to raise the level of digitalisation in these B-industries. The project’s approach was to match companies in health with relevant tech companies and provide funding so innovations could be developed.
“We see the medical sector, one of the most innovative sectors, is lingering behind in digitalisation.”
“We see the medical sector, one of the most innovative sectors, is lingering behind in digitalisation. When applying artificial intelligence to analysis of x-ray images, you can do much better diagnostics, statistical evaluations, and forecasts about who is disposed to get, for example, breast cancer. This is not just about making the processes more effective, but about the impact, which is better health, longer lives and saving lives,” said Tamara Högler, DIGI-B-CUBE coordinator on behalf of Oslo Cancer Cluster.
Made idea into prototype
In total, DIGI-B-CUBE provided 2,4 million euros in funding from the European Union’s Horizon 2020 Research and Innovation programme to 32 projects from 75 companies across Europe.
Cathrine Ro Heuch, CEO of Nordic Brain Tech, was one of the recipients. Heuch has suffered from headaches her entire life but received limited help from the healthcare system. When she met a group of neuroscientists with a novel solution while working for NTNU technology transfer, she decided to do something about it.
“The doctors from St Olav’s Hospital had invented a digital treatment for migraines in children. Using biofeedback, you can train the nervous system to be more relaxed. The principal of biofeedback is very old and recommended in the national guidelines for migraine treatments, but it is not available in the public healthcare system in Norway,” said Heuch.
Heuch founded the company Nordic Brain Tech with the goal to transform the solution into a product that is cost-effective and easy-to-use for patients at home. However, it is not easy to find private capital, because investors see a high risk in early-stage projects. Heuch needed public funding to make her idea into a prototype.
Högler also knows how difficult it is for early-stage companies to access public funding on an international level.
“Funding applications for European projects is not something you complete in one or two hours. It is a long process. The chance of receiving funding is low and the administrative process is complicated. In comparison, the application for DIGI-B-CUBE was quite lean and the project duration was short,” Högler explained.
Nordic Brain Tech applied for DIGI-B-CUBE funding, together with their partner i3tex in Sweden and their partner Thorgate in Estonia, and they were granted 150 000 euros.
“It was important to have partners in other countries because these skill sets are not widely available in Norway.”
“It was important to have partners in other countries because these skill sets are not widely available in Norway. There are many great medtech development companies in Sweden, so we found a partner there that could create the device. Estonia has many great software developers, so it was natural to ask someone there to help us create the app,” Heuch explained.
Using funding from DIGI-B-CUBE, they created a prototype that monitors body temperature, heart rate, and muscle tension, while connected to an app on your phone.
“The point of the treatment is to train the body to have better blood flow, increase the body temperature and relax the muscles in the neck. The idea is to follow a 12-week programme, using the product 10 minutes every day, to increase the patient’s awareness of how these body functions are connected to migraines,” Heuch explained.
Nordic Brain Tech are now on the way to launch a clinical study in Trondheim. If successful, this product may help the one in seven Norwegians who suffer from migraines today.

The DIGI-B-CUBE consortium met at Oslo Cancer Cluster in November 2021. From the left: Nikolaos Matskanis (Infopole), Panagiotis Markovits (Motivian), Gerry Renders (EISMEA), Miltiadis Anastasiadis (Motivan), Gawel Walczak (Secpho), Astrid Green (OCC), Milena Stoyanova (EISMEA), Ketil Widerberg (OCC) and Bente Prestegård (OCC).
Clusters connected companies
DIGI-B-CUBE was implemented by a consortium of eight partners in different European countries and co-ordinated by Oslo Cancer Cluster. The point of involving clusters was to ease the identification of the needs of the companies in each region and to simplify matchmaking between them.
“Small companies need incentives in order to work together across countries and sectors.”
“Small companies need incentives in order to work together across countries and sectors. It is great the European Union gives out these funds and that Oslo Cancer Cluster can take a role in connecting companies across Europe,” said Widerberg.
Carina Schachinger, Project Manager at Business Upper Austria, stresses that the success of the project went beyond the funding.
“This was a great success because we were able to connect these companies with research and business partners across borders. Companies could extend their network on an international level, which is normally quite difficult,” said Schachinger.
Although the corona pandemic made it challenging for the consortium and companies to meet, the interest in medical diagnostics suddenly increased. The fact that DIGI-B-CUBE went virtual enabled more companies from different countries to participate in the digital sessions. Ultimately, 980 SMEs applied for in total 426 innovation projects.
“What makes DIGI-B-CUBE great is that if you support these companies in their innovation, then it has an immediate benefit in the companies, but it is also about medical diagnostics and health in general. It has this big benefit for society. When we look at the 32 projects that received funding, it is great to have this precise approach to medicine and this can improve the lives for you and me,” said Schachinger.
Stay connected to our website and social media channels to learn more about our initiatives and funding calls on a European level.